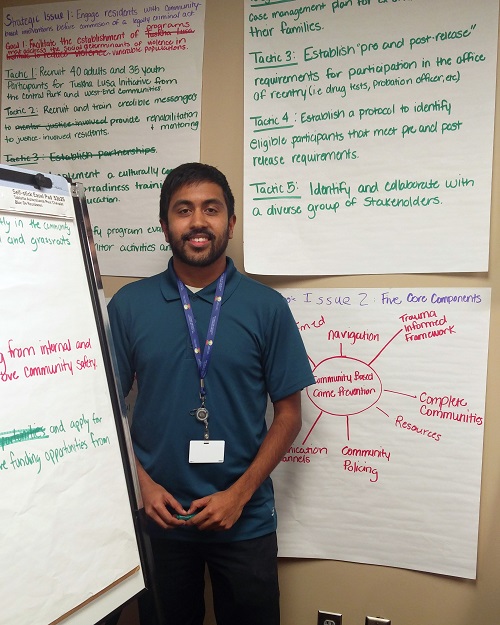
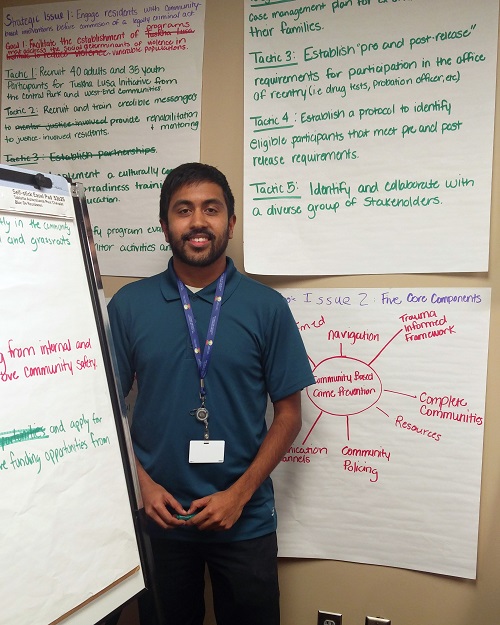
East Tennessee State University MPH candidate Matthew Barrett was in the middle of a field placement with the Tennessee Department of Health when the 2020 coronavirus pandemic hit the U.S. The Region IV Public Health Training Center interviewed him about this experience.
Tell us a little about yourself.
I am from Johnson City, Tennessee and I am completing my Master of Public Health at East Tennessee State University. I will be graduating this May! After graduation, I will continue to serve in the Army Reserves. I have been in the Army Reserves since 2008 and want to continue my Army Reserves career as an officer at the Army Public Health Center. In my civilian career, I want to continue working with the Tennessee Department of Health (TDH). I want to work directly with the people of Tennessee and be involved in formulating strategies and processes to getting systematic changes that lead to better performance measures and health outcomes for our communities.
Where are you completing your field placement? Who is your mentor?
I was placed at the TDH Northeast Regional Office. The most appealing aspect of this placement was my ability to work in the entire Northeast Region, encompassing seven counties and eight local health departments (LHDs). Traveling to and seeing the difference in how each LHD operates and meets the needs of its community is an amazing opportunity alone. That combined with working at each LHD location on process improvement is a unique and humbling learning opportunity. The differences between our largest county, Washington, and our most rural counties, Hancock and Johnson, really highlight the unique challenges faced in public health. Hancock County and Johnson County are both counties designated as Distressed Counties by Governor Lee. The ability to implement process improvement needs to be adjusted for the county, and the community itself is also organized very differently, requiring an adjustment to strategies to get the community involved in public health initiatives. My placement allowed me to see this firsthand across the Northeast Region.
My mentor at the Northeast Regional Office has been Kristen Spencer, the Assessment and Planning Coordinator and Press Information Officer. Kristen and other staff have been instrumental in my success and learning during this field experience. My mentors not only provided me opportunities to learn but also took their time to coach me. I can’t thank them enough for the professionalism and kindness shown to me.
What projects were you originally working on?
Before the pandemic began, I was involved in a clinical performance improvement project. I was organizing the project and leading it. I had another student, Olufeyisayo Odebunmi, who was also doing her field experience at the Regional Office. She helped tracked patients and is now currently doing analysis on the clinics that we completed and got all the data from. The project involved following patients through our primary care and general clinics. The goal of the project was to create visual representations of a patient’s visit in order for staff to easily identify step they could take to reduce patient wait time, increase the speed of current processes, or justify future changes to reduce cycle times and increase the time patients spent with providers. Along with these visual maps we also collected massive amounts of data that include, cycle times, patient show rates, time spent with staff, time spent walking between rooms, time spent waiting at specific points in the visit.
How have things changed with your field placement since the pandemic? What role have you had in assisting with COVID-19 response?
When the pandemic began, TDH entered its Continuity of Operations Plan and all nonessential activities ceased. This included our project. When the COVID-19 crisis began, our Regional Health Operations Center (RHOC) was activated, and we began by calling in the Medical Reserve Corps to help staff an informational line. I helped staff the informational line. I also had the opportunity to work as the logistics officer for a day. I helped process requests by organizations for personal protective equipment (PPE). The PPE is distributed by the Northeast Healthcare Coalition. The request is taken by the RHOC logistics officer and is then processed for voting on by the coalition. Being involved on crisis management during my field experience is not something I expected, but it was valuable to see how information flowed during the event.
My most significant project during the crisis was to create a method to reach out to contacts of individuals with confirmed COVID-19. Dr. Kirschke, the Northeast Regional Medical Director, came up with an idea to use automated text to reach out to the case-contacts. I made this happen by working with the investigators and using existing resources to create a simple and easy to use method of sending daily text messages to case-contacts. The contacts received the daily reminder until they reached 14-day point of quarantine and after having no more contact with the confirmed case. The reminder also included a phone number to our providers if a case-contact began to show symptoms of COVID-19. After creating this method, I sent it up our leadership chain so that other regions can also utilize the same method if desired.
How has this experience affected you?
Overall, this has been the most significant learning opportunity of my graduate education. I am looking forward to entering public health after graduation, but I do hope that this crisis ends soon. While it was a valuable experience to see public health emergency resources in action, I want to be back to working on process improvements and community engagement in public health. This crisis has furthered cemented my desire to continue working in this field.