by R-IV PHTC | Apr 19, 2021 | Training
Opioid Use Disorder Treatment During COVID-19: Challenges and Opportunities
Year: 2021 | Competency/Strategic Skill: Program Planning | Priority Topic: Opioid Abuse | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a live webinar held on April 28, 2021. This webinar is co-sponsored by the Injury Prevention Research Center at Emory.
The epidemic of opioid use and related harms has been exacerbated by the ongoing COVID-19 pandemic. Mitigation strategies for COVID-19 have led to disruption in the delivery of healthcare, increased social isolation, and rapid release of individuals from jails and prisons- all of which may increase the risk of overdose. Gaps in the continuum of care including access to mortality-reducing medication treatment for opioid use disorder have become more evident. In response, the federal government has made significant changes intended to provide more flexibility in how and where care is delivered for both methadone and buprenorphine treatment. Providers have welcomed these changes, and we will discuss several of these practice changes including how to utilize telemedicine and new long-acting injectable formulations to initiate and help retain patients in care.
by R-IV PHTC | Apr 19, 2021 | News
Recent and ongoing horrific incidents in our country have drawn renewed attention to the fact that racism is not only a public health issue, but a public health crisis. The Emory University and the Rollins School of Public Health communities have been swift to respond with statements from leadership and student organizations, vigils and commemorations, resource and reading lists, and educational events.
Here at the Region IV Public Health Training Center, we, too, acknowledge that systematic racism and racist violence continue to hurt our communities and that we are responsible for working to address these tough issues. Specifically, we have taken these steps:
The Region IV Public Health Training Center Anti-Bias and Anti-Racism Commitment
Many of the greatest ideas and discoveries come from a diverse mix of minds, backgrounds and experiences. As a reminder, the Region IV Public Health Training Center welcomes diverse and inclusive interactions and comments from our participants. It is how we learn best. When participating in our trainings, please be respectful of others. Racism, discrimination, microaggressions or hate in any form will not be tolerated. Thank you for helping us sustain a safe, inclusive and respectful learning community.

by R-IV PHTC | Apr 15, 2021 | Field Placement Stories
Christina Faulk was an MPH candidate at the Medical University of South Carolina when she served as a Region IV PHTC Pathways to Practice Scholar in the fall of 2020. As a research intern at the South Carolina Department of Health and Environmental Control (DHEC), Christina assessed childhood homelessness as a risk factor to opioid misuse and the role of effect modifiers as protective factors. Here is Christina’s reflection on her experience in her own words:
I chose this field placement because I knew that statistics was not one of my strengths and I wanted to build my skills in SAS and statistical analysis. My field placement gave me more experience in this subject matter and I was extremely fortunate to be able to work with the Director of Surveillance at DHEC, who is very knowledgeable in the field of Epidemiology, and Research and statistics.
I learned that with good public health research, a huge impact can be made for an entire population of people, which is quite profound. My mentor taught me patience, to believe in myself, and with dedication and effort anything can be accomplished. I have grown both personally and professionally during this field placement and feel more confident with large datasets and my ability to use statistical programing software to clean and analyze data.
This opportunity has confirmed my desire to work with data and research, specifically trauma and substance abuse research. I am extremely grateful and fortunate to have had this experience and encourage all public health graduate students to apply to the Pathways to Practice Scholars field placement.

by R-IV PHTC | Apr 12, 2021 | Training
Healer, Heal Thyself: Tools for Wellness and Self-Care during the COVID-19 Pandemic
Year: 2021 | Competency/Strategic Skill: Change Management | Priority Topic: Mental Health | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a live webinar held on April 20, 2021.
During this webinar, we will focus on helping public health professionals develop tools needed to enhance their self-care and overall wellness. Approaching wellness from a holistic perspective, participants will leave with actionable items to develop a plan for self-care. The objective is to increase the investment in their personal wellness and self-care while becoming an example for those they serve. This webinar will teach them how to relieve the stresses they face in healthy ways and help them identify mental health resources and natural supports.

by R-IV PHTC | Apr 1, 2021 | Featured Training, Training
Using Message Framing Tools to Build and Sustain Cross-Sector Partnerships
Year: 2021 | Competency/Strategic Skill: Community and Partner Engagement | Priority Topic: N/A | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 30-minute self-paced online module. This is the second of three courses about Public Health Reaching Across Sectors (PHRASES).
This course focuses on the 10 PHRASES (Public Health Reaching Across Sectors) framing recommendations and four framing tools. The four framing tools included in the PHRASES Toolkit are frame elements, sample emails, “When You Say They Think” charts, and reframed answers to tough questions.

by R-IV PHTC | Mar 19, 2021 | Training
Purpose Built Communities and the Role of Public Health
Year: 2021 | Competency/Strategic Skill: Leadership and Systems Thinking | Priority Topic: N/A | Setting: On-Demand | Format: Live | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on March 31, 2021.
During this webinar, we will discuss the causes and impact of poverty as well as the role of public health in building cross-sectoral partnerships to improve social determinants of health. We will discuss the Purpose Built Community approach to building healthier communities and more equitable neighborhoods and the impact COVID-19 is having on the community development strategies.

by R-IV PHTC | Mar 19, 2021 | Training
At-Risk Adult Abuse: Hiding in Plain Sight
Year: 2021 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: Mental Health | Setting: Online | Format: Live | Sponsor: Emory University/Central Office
Overview:
This is a live webinar scheduled for April 7, 2021 at 9am ET. This webinar is co-sponsored by the Injury Prevention Research Center at Emory.
Learn how to recognize signs of elder abuse in a healthcare setting by better understanding Abuse, Neglect, and Exploitation (ANE) and related policies.
by R-IV PHTC | Mar 10, 2021 | News
by R-IV PHTC | Mar 10, 2021 | News
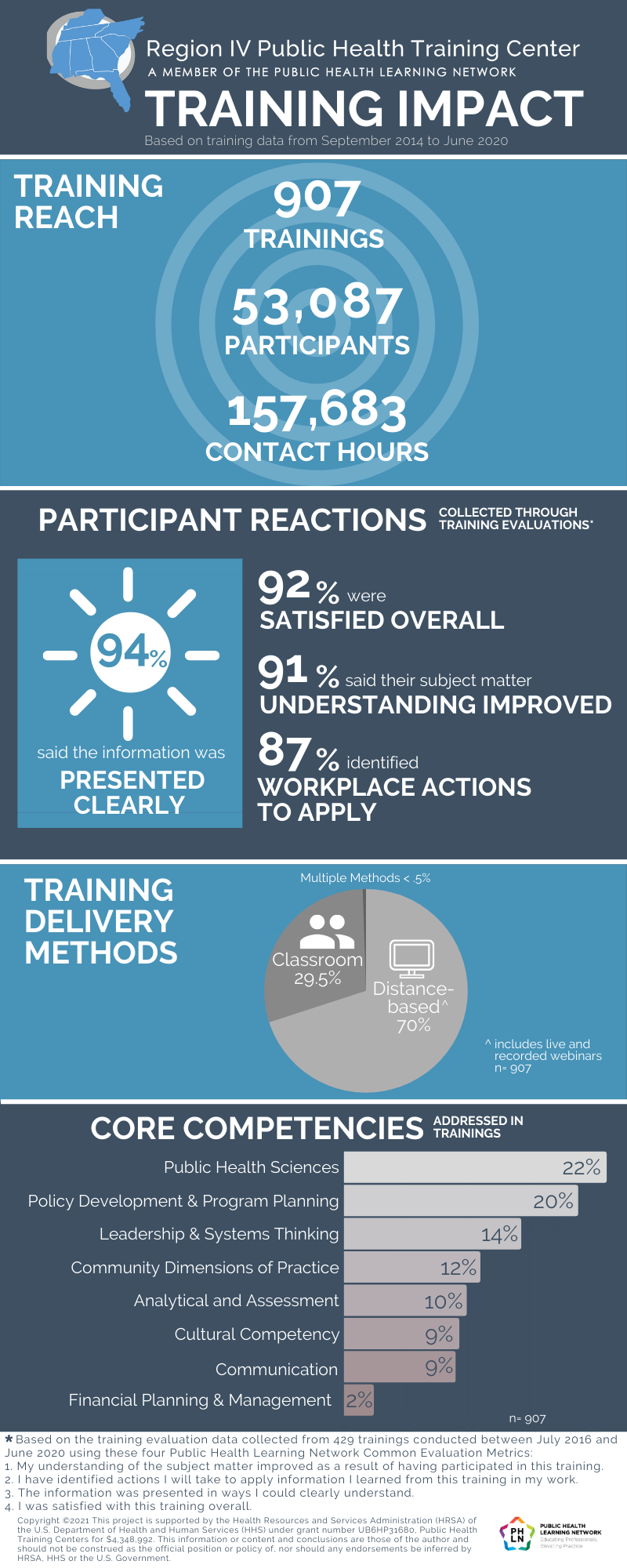
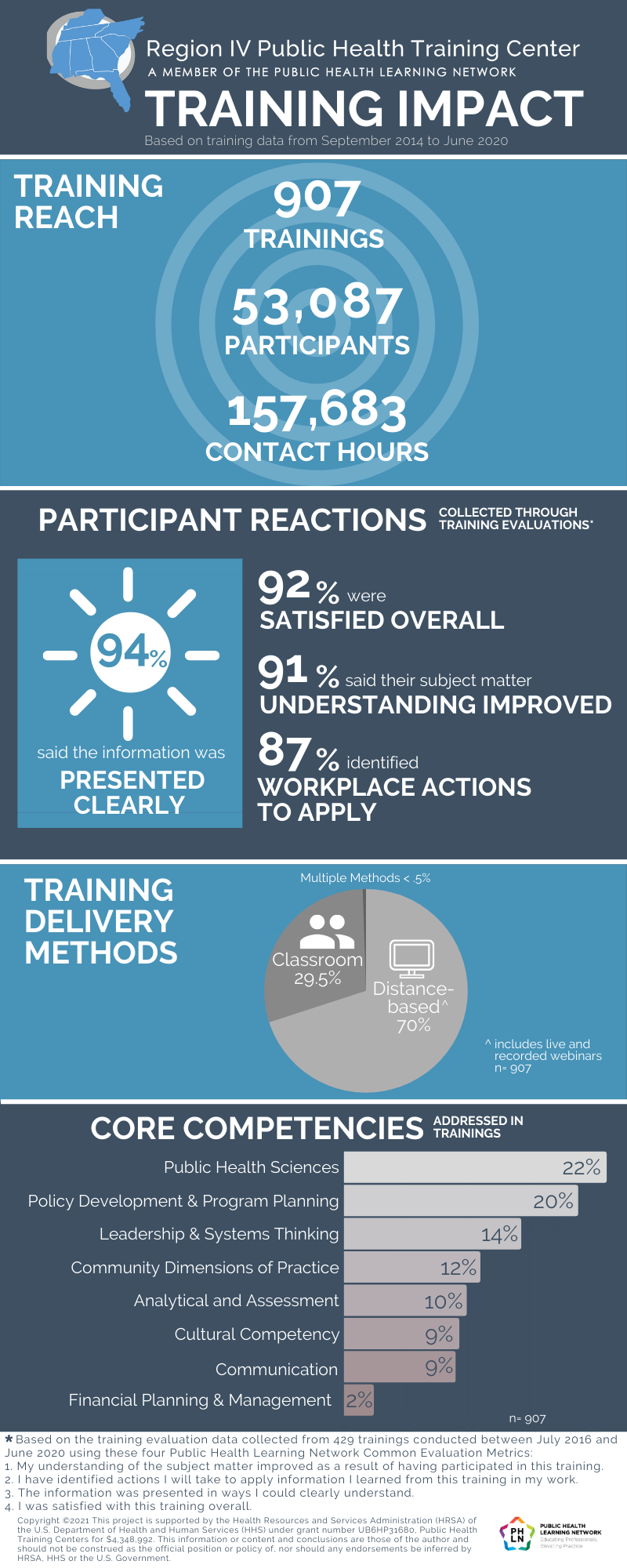
The Region IV Public Health Training Center is committed to measuring the impact of our training programs on the public health workforce. The infographic below provides an overview of the reach and evaluation findings from trainings held between September 2014 and June 2020.

by R-IV PHTC | Mar 3, 2021 | Training
COVID-19 Pandemic and the Isolated Child: Risks and Stressors
Year: 2021 | Competency/Strategic Skill: Community and Partner Engagement| Priority Topic: Other Infectious Diseases | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on March 15, 2021.
During this webinar, we will address a variety of issues facing children and families during the pandemic including risks due to social isolation, virtual schooling, and the added stress on families. It will discuss how to help children adjust to being back to in-person school and stressors they may be experiencing. Resources will be provided to support children and families.

by R-IV PHTC | Feb 26, 2021 | Featured Training, Training
Leading Change in Informatics and Data Analysis
Year: 2021 | Competency/Strategic Skill: Data Analytics and Assessment| Priority Topic: N/A | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Change is a constant in both our personal and professional lives. The idea that human beings naturally resist change is deeply ingrained into our culture and how we think about change. This course provides public health professionals with a foundation in change management and practical tools for utilizing formal change management for an informatics or data analytics project.
The entire training is expected to take 30 minutes to complete. There are no prerequisites.
The course contains three modules: the content module, a workbook, and an evaluation. After finishing all three modules, learners will earn a certificate of completion. When the certificate is available, learners will see a Certificate button on their dashboard.
Participants will need a broadband internet connection (Google Chrome or Mozilla Firefox are preferred browsers) and computer speakers. For technical support, please contact emoryphtc@emory.edu.

by R-IV PHTC | Feb 26, 2021 | Training
Health Equity: Marriage of Programming and Policy
Year: 2021 | Competency/Strategic Skill: Policy Development| Priority Topic: N/A | Setting: Online | Format: Live | Sponsor: University of North Carolina, Wilmington
Overview:
This is a live webinar scheduled for March 9, 2021 at 9am ET.
Join us for an insightful conversation about the intersection of programming and policy development with a focus on nutrition access and infant and maternal health. Dr. Deidre Grim of Healthy Savannah and Grim Consulting Group joins us from a city that mirrors our own. Savannah, Georgia, is a port city that faces similar challenges with nutrition access and infant and maternal health. In this session, we will explore how she navigated both challenges in her work within the nonprofit Healthy Savannah, and her experiences with First Food Friendly Communities. She has learned that in order to make sustainable and equitable change, one must co-develop programming that will lead to lasting policy change. Dr. Grim lives by the words of Vice President Kamala Harris teaches, “If you are fortunate to have an opportunity, it is your duty to make sure other people have those opportunities as well.”
Joining her in this conversation is Marissa Bryant Franks, Health Equity Outreach Coordinator for New Hanover Regional Medical Center, and Evan Folds, Project Manager, Northside Food Co-Op and Founder/President of Be Agriculture. Get ready for an engaging interview-style conversation between leaders in two similar port cities. Hosted by Center for Healthy Communities and NC Public Health Training Center, part of UNCW CHHS Community Engagement.

by R-IV PHTC | Feb 16, 2021 | Featured Training, Training
Racism, Bias, and Other Determinants of Health: Issues and Actions
Year: 2021 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion| Priority Topic: N/A | Setting: On-Demand | Format: Live | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a live webinar.
During this webinar we will discuss racism and social determinants of health, and the role bias plays in healthcare decision making as well as its impact on adverse health outcomes. We Weill discuss how our backgrounds inform our perspectives and how we relate to colleagues and patients. We will also explore strategies that students and physicians can employ to mitigate bias.

by R-IV PHTC | Feb 10, 2021 | Training
Bridging Mental Health and Public Health During COVID-19: A Town Hall
Year: 2021 | Competency/Strategic: Community and Partner Engagement | Priority Topic: Mental Health | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a live webinar. The Southeast Mental Health Technology Transfer Center (MHTTC) co-sponsored this webinar.
The COVID-19 Pandemic has placed both mental health and public health workers on the front lines in an array of on-going stressful situations. As a result, mental health and public health agencies have had to innovate and adapt practices to support and care for their workforce and the populations they serve. This townhall event will feature mental health and public health agency representatives sharing insight on ways they have addressed COVID-19 while also supporting staff, the value of Mental Health-Public Health partnerships, and the related challenges they anticipate during the first half of 2021. Our panelists for this event include Dr. Audrey Arona, Chief Executive Officer and District Health Director for the Gwinnett-Newton-Rockdale County Health Department, and Jennifer Hibbard, Chief Executive Officer for Viewpoint Health.

by R-IV PHTC | Feb 2, 2021 | Training
COVID-19 Vaccine Hesitancy
Year: 2021 | Competency/Strategic Skill: Program Planning| Priority Topic: Other Infectious Diseases | Setting: Online | Format: Live | Sponsor: Medical University of South Carolina
Overview:
This is a live webinar scheduled for Friday, February 19, 2021 from 12pm-1pm ET.
The Medical University of South Carolina Department of Public Health Sciences is hosting a Public Health Training Web Series. This webinar will focus on COVID-19 vaccination hesitancy. The presenter will be Dr. Danielle Scheurer, Professor of Quality Management and Patient Safety at the Medical University of South Carolina.

by R-IV PHTC | Jan 27, 2021 | Training
Racial Disparities at Every Stage of COVID-19: Infections, Hospitalizations, Death Rates… and Now the Vaccine
Year: 2021 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on February 8, 2021.
During this webinar we will discuss how the existing racial disparities and health inequities in our country have amplified the effects of COVID-19. From infection rates, hospitalizations, and deaths, communities of color have been impacted by COVID-19 at higher rates. Now, after more than a year since the world woke to a spreading viral pandemic, an effective COVID-19 vaccine offers protection and a promise of normal life. But a final-step challenge persists – getting the vaccine into the arms of people who need it most. Please join us for a presentation and conversation with Taison Bell, MD and moderated by Sam Fulwood, PhD.

by R-IV PHTC | Jan 19, 2021 | Featured Training, Training
Dynamic Education And Learning (DEAL)
Year: 2022 | Competency/Strategic Skill: Program Planning| Priority Topic: N/A | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
These are recordings of our 5-session series of 90-minute interactive online workshops offered every other week starting March 10, 2022 and ending May 5, 2022. All sessions were from 1–2:30 pm ET. Learners may choose to register for all workshops in the series or for individual sessions.
Dynamic Education And Learning (DEAL) is designed for public health professionals who want to elevate the quality of the distance-based trainings they develop and deliver. The series covers training planning, promotion, implementation and evaluation. Although much of the content is developed with distance-based training in mind, many concepts can also be applied in in-person trainings as well. Learners can register for any or all of the five sessions.
Session 1 Best Practices for Developing Quality Distance-based Training covers key terminology, e-learning standards, best practices and unique considerations for engaging in the distance-learning environment.
Session 2 Developing a Strong Foundation for Your Training covers how to define and learn about a target audience, develop learning objectives, create appealing titles and descriptions, and ways to promote training offerings.
Session 3 Introduction to Technology for Teaching and Assessment covers technology tools and the selection of appropriate strategies and technologies for teaching and assessment.
Session 4 How to Create Engaging Webinars and Interactive Slideshows covers webinars and interactive slideshows, and discusses the value of interaction in adult learning and how technology can be used to engage learners.
Session 5 Developing Training Evaluations covers methods of evaluation, Kirkpatrick’s levels of evaluation, effective survey questions, and strategies of data collection.

by R-IV PHTC | Jan 12, 2021 | Training
One RNA Virus is Enough! HIV Care in the Setting of the COVID Pandemic
Year: 2021 | Competency/Strategic Skill: Leadership and Systems Thinking | Priority Topic: HIV/AIDS | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is 90-minute recording of a webinar held on January 21, 2021.
During this webinar, we will review how the COVID-19 pandemic has detrimentally affected HIV care and steps that have been taken to mitigate these effects.
by R-IV PHTC | Jan 11, 2021 | News
Today’s public health challenges, like climate change and COVID-19, are complex and require public health professionals to lead large-scale changes that no one person can solve alone. They also require an adaptive public health workforce with diverse knowledge and skills to respond to evolving issues, engage in collective learning, and intervene at organizational, community, and systems levels.
The Public Health Learning Network acknowledges the enormity of this task and has developed a new framework and other tools for doing the work. You can find it all in their new resource, Creating a Learning Agenda for Systems Change: A Toolkit for Building an Adaptive Public Health Workforce.
Recognizing that individual skill building is important but often insufficient for supporting an adaptive workforce, the toolkit helps leaders think beyond training for individual competencies and instead facilitate organizational learning in response to community health needs. The framework embedded in the toolkit helps workforce specialists understand and define public health problems, align the problem with the type of change needed to address it—like increasing knowledge or addressing social norms—and recommend complementary learning strategies to tackle the problem with a vision of addressing systems change.
The toolkit also includes problem-solving tools for moving these concepts into action. The rapid self-assessment helps organizations identify community challenges and examine their current learning state to address them. The discussion guide helps leaders facilitate conversations as they move through each step of the framework. And the learning approach planning tool assists in designing learning opportunities that best fit the community challenge and desired level of impact.
“We want public health leaders and their partners to use this toolkit as a catalyst for their design thinking and planning to change the way their organizations approach learning. This is critical for building learning strategies that can facilitate more ongoing innovation in today’s public health workforce,” said Christina Welter, DrPH, MPH, lead author of the toolkit and associate director for the Policy, Practice, and Prevention Research Center at the University of Illinois at Chicago School of Public Health.
Are you ready to take your organization’s training and learning to the next level? Visit the Public Health Learning Agenda and download a copy of the toolkit today.
Interested and want to know more before you begin? View the on-demand kick-off webinar to hear more about how these concepts and tools fit together and about future pilot testing for the toolkit.
The Public Health Learning Network is a national coalition of 10 Regional Public Health Training Centers and their partners organized to meet public health workforce development needs.

by R-IV PHTC | Jan 7, 2021 | Training
Creating a Learning Agenda for Systems Change: A Toolkit for Building an Adaptive Public Health Workforce
Year: 2021 | Competency/Strategic Skill: Leadership and Systems Thinking | Priority Topic: N/A | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a recording of a one-hour webinar held on February 2, 2021.
Many complex and systemic challenges such as racism, the opioid crisis and mental health stand at the root of community health issues. These are challenges that no individual can address alone, and no single solution or intervention will solve. Therefore, the public health workforce needs to have the knowledge and skills to respond adaptively and to engage in multi-sector collaborations and multi-level interventions. Existing public health workforce development models, however, largely address gaps in specific skills or content areas of individual learners and individual competencies.
The Public Health Learning Network (PHLN) has developed the Learning Agenda Toolkit to help the public health workforce develop a coordinated system of effective, efficient and quality learning to address complex challenges. The Creating a Learning Agenda for Systems Change: A Toolkit for Building an Adaptive Public Health Workforce includes a conceptual Learning Framework, Rapid Assessment Tool, Discussion Guide, and Learning Approach Planning Tool to help public health leaders and workforce development specialists build a robust Learning Agenda and achieve their vision of systems change. The purpose of this presentation is to provide an overview of the Learning Agenda Toolkit and how different Learning Approaches – implemented over time – can be used to build collective competency to address community challenges. The session will also include a discussion of some ways that public health leaders might use the Learning Framework and tools to better align Learning Opportunities to address their communities’ challenges.
This webinar will be co-presented by Christina Welter, DrPH, MPH and Karla Todd Barrett, MBA, MSM. Dr. Welter is a policy practitioner, visionary leader, and practice-based researcher committed to helping organizations and their partners co-create equity-focused systems change. Among many roles, she is the Director of the DrPH in Leadership at the University of Illinois at Chicago School of Public Health. Ms. Todd Barrett is the Senior Program Manager and Training Specialist at the Boston University School of Public Health. She manages overall operations and partnerships for the New England Public Health Training Center (NEPHTC), including training delivery and development, data analysis, and governance.
To download your copy of the Learning Agenda Toolkit, please go to www.publichealthlearningagenda.org.

by R-IV PHTC | Jan 5, 2021 | Training
Impact of Child Sexual Abuse: Empowering Prevention through Education
Year: 2021 | Competency/Strategic Skill: Program Planning | Priority Topic: Mental Health | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on January 11, 2021.
Child sexual abuse prevention starts with knowledge and awareness of the problem. This webinar provides professionals who work with children and families with an overview of the issue as well as tools and strategies to create safer environments for children in both a professional and personal setting. The webinar will cover practical actions adults can take to reduce instances of child sexual abuse in their organizations, families, and communities, and will give participants information about evidence-informed training programs available to deepen knowledge and enhance skill building to prepare adults to speak up and prevent sex abuse.
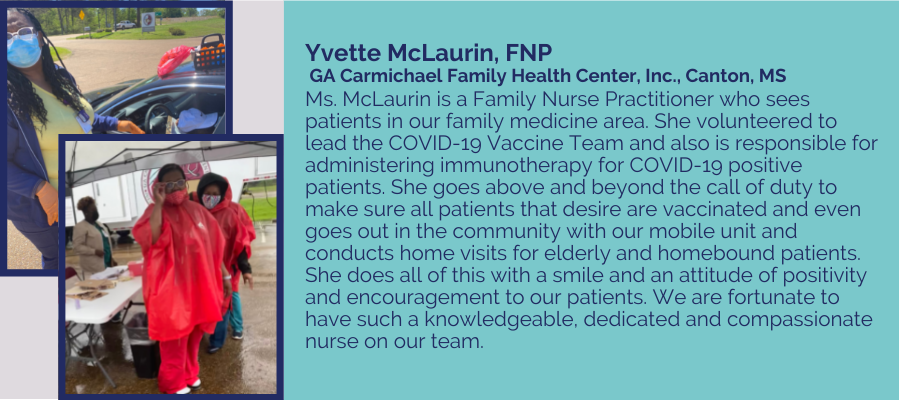
by R-IV PHTC | Dec 15, 2020 | Archive, News
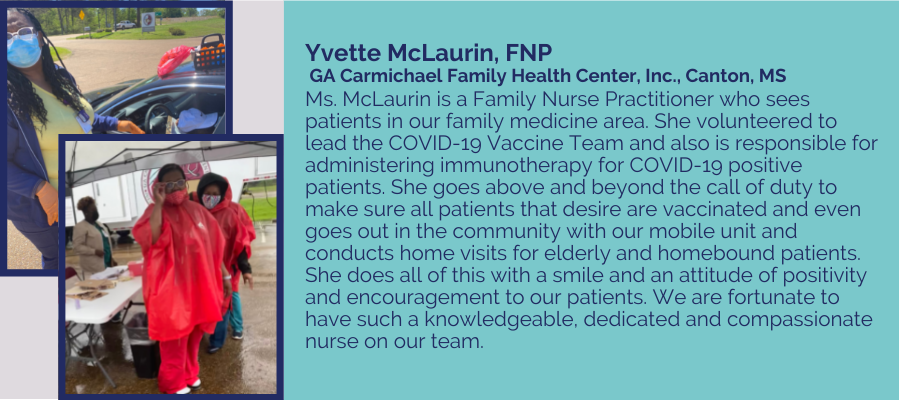
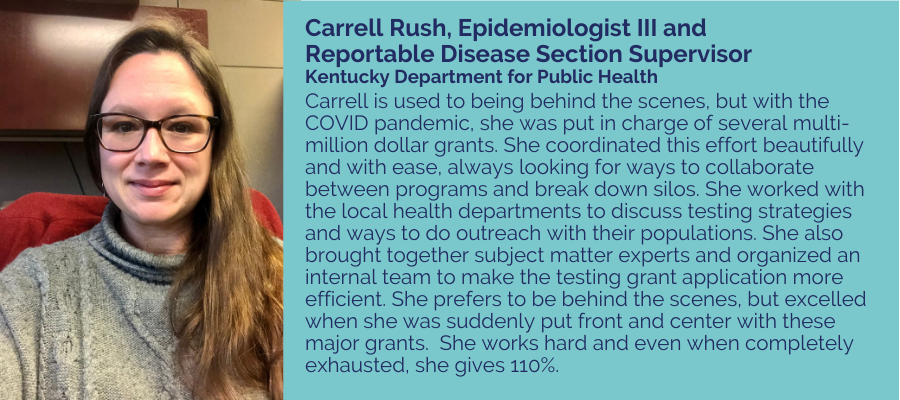
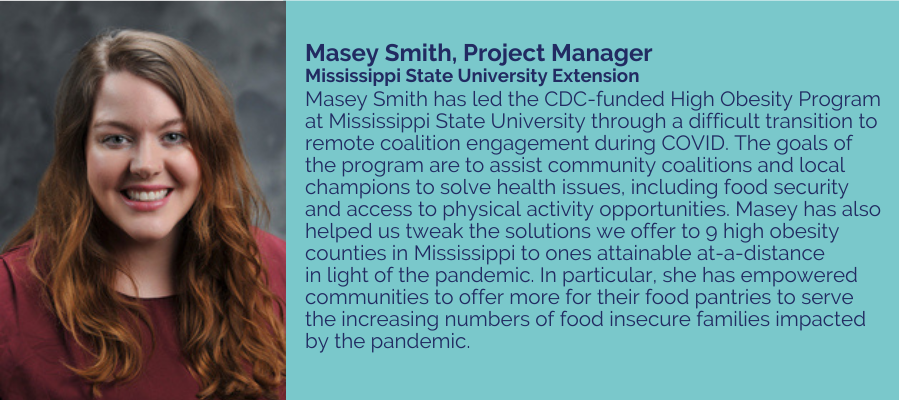
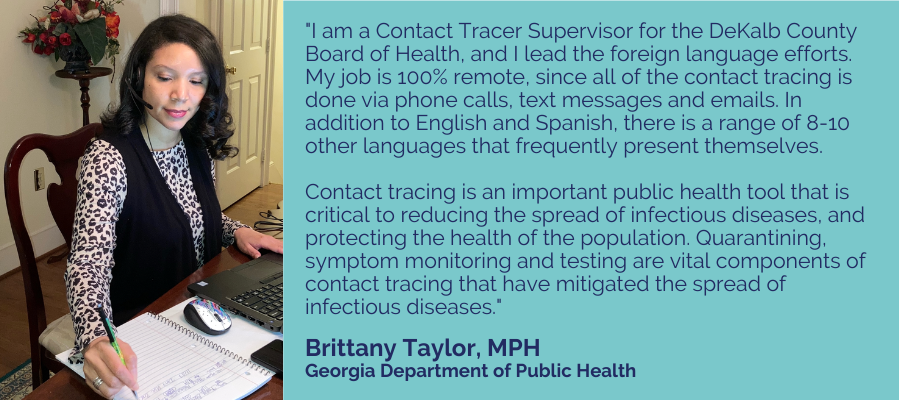
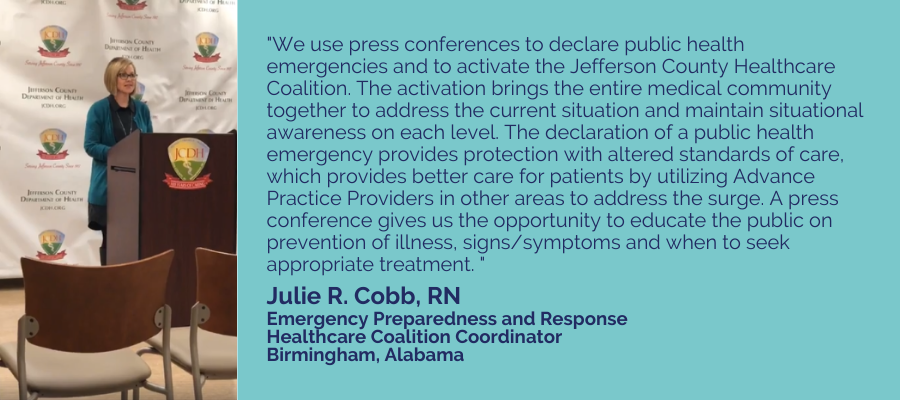
The COVID-19 pandemic has heightened both awareness and scrutiny of the field of public health. Public health professionals have been tasked with responding to the virus in a highly politically charged environment, while also continuing to provide regular programs and services in the challenging circumstances of a pandemic. As a county health department Community Coalition Coordinator explained:
Our health department is handling all things COVID for the county—testing; providing guidance to schools, businesses, employers, agencies, health care providers and the public; investigating and enforcing of state regulations; contact tracing; providing lab results to EVERY single person who takes a COVID test; arranging and providing a multiplicity of testing events that change weekly to meet the current need; and monitoring and assisting people placed in quarantine/isolation to make certain they have what they need and do not violate the order. We also provide shelter and housing and food for people who have no safe place to quarantine or isolate. As employees of the health department we are considered first responders and throughout this crisis are constantly being pulled away from our regular work. I have so much work to do and so very little time. Just because COVID-19 came to town does not mean all of the other health problems went away.
In this new photo blog, Portraits of Public Health, the Region IV Public Health Training Center seeks to highlight and appreciate the folks who have been and continue to do the hard work of public health. To nominate a public health professional to be included, please use this form. Priority will be given to nominees from Region IV.

by R-IV PHTC | Dec 2, 2020 | Training
Vaccine Hesitancy among African American Communities
Year: 2020 | Competency/Strategic Skill: Cultural Competence, Diversity, and Inclusion | Priority Topic: Other Infectious Diseases| Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on December 16, 2020.
Vaccine refusal or delay has substantial public health implications. During this webinar, we will discuss vaccine hesitancy among African American communities. We will discuss the history of vaccine hesitancy and how we can build trust in the African American community to increase vaccine uptake. At the end of this webinar, participants will be able to: a) define vaccine hesitancy, b) describe racial disparities in vaccine coverage, c) describe approaches to overcome vaccine hesitancy.

by R-IV PHTC | Dec 1, 2020 | Featured Training, Training
An Overview of Public Health Reaching Across Sectors
Year: 2020 | Competency/Strategic Skill: Community and Partner Engagement | Priority Topic: N/A | Setting: online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 30-minute online course. This is the second of three courses about Public Health Reaching Across Sectors (PHRASES).
This online course is an overview of Public Health Reaching Across Sectors or PHRASES, a compilation of communication strategies and tools for public health professionals to use to foster a better understanding of public health and the greater willingness of other sectors to engage in cross-sector partnerships. It will provide an introduction to how productive framing and messaging can improve partnerships and overall health outcomes, and an overview of the tools and strategies PHRASES provides to improve communication to other sectors.
PHRASES is a joint project of the de Beaumont Foundation and the Aspen Institute’s Health, Medicine and Society Program.

by R-IV PHTC | Nov 5, 2020 | Training
Systemic Racism and Health Disparities: The Impact of COVID-19 on Latinx Populations
Year: 2020 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on November 11, 2020.
During the COVID-19 pandemic, long-standing systemic health and social inequities have been exposed and certain populations are at an increased risk of the impacts of COVID-19. During this webinar we will discuss how systemic racism has historically prevented Latinx communities from adequate healthcare and other economic opportunities. We will discuss the impact COVID-19 is having on the Latinx community and how we must look at the systemic issue of race and health disparities as we move forward.

by R-IV PHTC | Nov 3, 2020 | Training
Psychological Impact of Hate Crime and Mass Violence
Year: 2020 | Competency/Strategic Skill: Community and Partner Engagement | Priority Topic: Mental Health| Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on Thursday, November 19, 2020. The Injury Prevention Research Center at Emory co-sponsored this webinar.
This webinar will provide an overview discussion of current definitions of mass violence incidents (MVIs) and hate crimes, impact on victims and communities, as well as current best practices in preparing for and responding to MVI events. Participants will learn about short-term and long-term approaches to assisting communities in healing after a MVI or hate crime that has impacted a broader community. In addition, participants will be provided a brief overview of the latest resources available from the National Mass Violence Victimization Resource Center (NMVVRC) which was established in October of 2017 in partnership with the Office for Victims of Crime (OVC) within the Office of Justice Programs, U.S. Department of Justice. The webinar will be presented by Alyssa Rheingold, PhD, Associate Director of Administration and Director of Clinical Operations at the National Crime Victim’s Research and Treatment Center (NCVC) within the Department of Psychiatry and Behavioral Sciences at the Medical University of South Carolina.

by R-IV PHTC | Oct 12, 2020 | Training
Communicate Effectively While Wearing a Mask and in Virtual Environments
Year: 2020 | Competency/Strategic Skill: Communication | Priority Topic: Other Infectious Diseases | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on October 26, 2020.
As we begin discussions of re-opening the nation, we are all faced with the reality of walking back into a world that is vastly different than just a few months ago. Perhaps most noticeably, many public places have initiated mask policies. In a recent study completed in Hong Kong, it was determined that wearing a mask can decrease infection by 75%. In short, by wearing a cloth mask you significantly reduce your own risk of exposure to and spread of virus containing particles. Wearing a mask can be an effective protective measure in preventing community spread of COVID-19, however, we can’t ignore its effects on day to day life. Masks are annoying, uncomfortable, and inconvenient, especially when you need to vocally communicate while wearing one. The workforce is also moving towards virtual platforms in with thunderous acceleration. Virtual platforms also create challenges for communication from home-office ergonomic blunders to prolonged conference calls with less than superb equipment.
This webinar is purposed to equip a diverse, public-facing group of professionals with information and skills necessary to overcome these communication barriers with excellence. Topic areas will include the anatomy and physiology of communication, purposeful enhancement of communication techniques to overcome physical and digital barriers, and recovery techniques to combat work and life related vocal fatigue. The webinar will be presented by Nathaniel Sundholm, MS, CCC-LSP, of the Emory Voice Center.

by R-IV PHTC | Oct 8, 2020 | Training
Stemming the Rising Tide of STDs through Partnerships and Comprehensive Strategies
Year: 2020 | Competency/Strategic Skill: Community and Partner Engagement | Priority Topic: Other Infectious Diseases | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on Monday, October 19.
This presentation will cover the rising rates of STDs in the United States, drivers of these rates and innovative approaches to mitigate these trends. The role of STDs in Ending the HIV Epidemic (EHE) and the impact of COVID-19 on STD trends will also be discussed. The webinar will be presented by Gail Bolan, MD, Director of the Division of STD Prevention at the Centers for Disease Control and Prevention.

by R-IV PHTC | Oct 2, 2020 | Training
Cultivating Cultural Humility in Public Health Practice
Year: 2020 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: N/A | Setting: Online | Format: Live | Sponsor: Medical University of South Carolina
Overview:
This is a live webinar scheduled for Friday, December 4, 2020 at 12:00pm ET.
The webinar will be presented by the Medical University of South Carolina Department of Diversity, Equity, and Inclusion.
by R-IV PHTC | Oct 2, 2020 | Training
HIV/AIDS in South Carolina
Year: 2020 | Competency/Strategic Skill: Data Analytics and Assessment | Priority Topic: HIV/AIDS | Setting: Online | Format: Live | Sponsor: Medical University of South Carolina
Overview:
This is a live webinar scheduled for Friday, November 13, 2020 at 12:00pm ET.
The webinar will be presented by Virgina Fonner, PhD, MPH, Assistant Professor of the Division of Global and Community Health at the Medical University of South Carolina.

by R-IV PHTC | Sep 24, 2020 | Training
Making Sense of COVID-19 Data
Year: 2020 | Competency/Strategic Skill: Data Analytics and Assessment | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This webinar with Amber Schmidtke, PhD, was held on September 30, 2020.
Public health data are often imperfect, which means we have to rely on multiple data streams to get a clearer picture of the present situation. Proper understanding of data with context is the antidote to disinformation. In this webinar, we’ll go through how to find and evaluate data, identifying the merits and challenges of different data sets, to make sure we have the right data to answer our questions.

by R-IV PHTC | Sep 15, 2020 | Training
Ending the Silence for Families
Year: 2020 | Competency/Strategic Skill: Community and Partner Engagement | Priority Topic: Mental Health | Setting: Online | Format: Live | Sponsor: Emory University/Central Office
Overview:
This is a live webinar scheduled for September 23, 2020 from 10-11am ET. This webinar is co-sponsored by the Injury Prevention Research Center at Emory.
Join us as we discuss mental illness warning signs, facts and statistics. Guest presenters Annie Connor and Lauren Paul are with NAMI (National Alliance on Mental Illness) Georgia.

by R-IV PHTC | Aug 26, 2020 | Training
Unexplained Pediatric Deaths: Investigation, Certification, and Family Needs: Procedural Guidance and Key Considerations Developed by the National Association of Medical Examiner’s Panel on Sudden Unexpected Death in Pediatrics
Year: 2020 | Competency/Strategic Skill: Data Analytics and Assessment | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-Demand | Sponsor: Alabama Public Health Training Network, Alabama Department of Public Health
Overview:
This is a 60-minute recording of a webinar held on September 4, 2020.
The workshop focuses on the medicolegal investigation of sudden, unexpected pediatric deaths, focusing on those deaths which remain incompletely understood or entirely unexplained. It discusses the evolution of our understanding and practice in the area of sudden, unexpected pediatric death investigation. Procedural guidance for investigation, certification and reporting, and key considerations for prevention and working with family members and other professional team members are provided.
by R-IV PHTC | Aug 26, 2020 | Archive, News
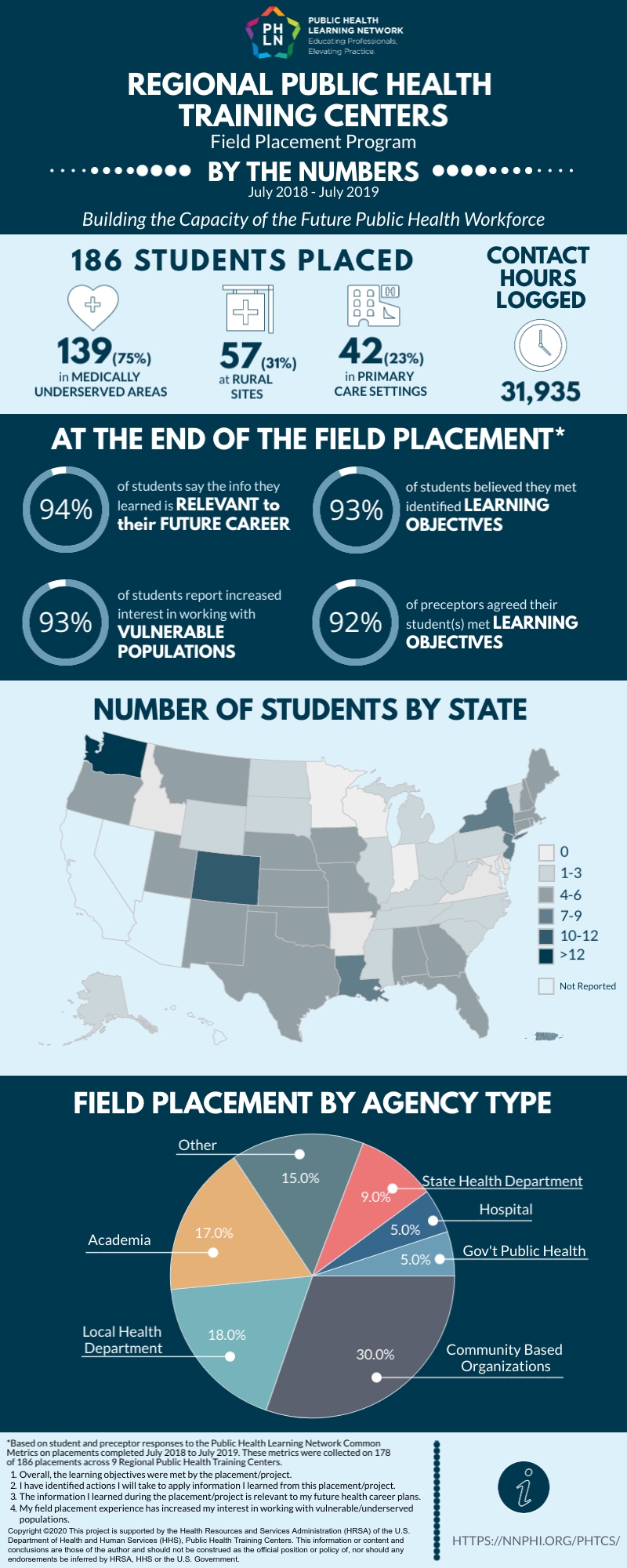
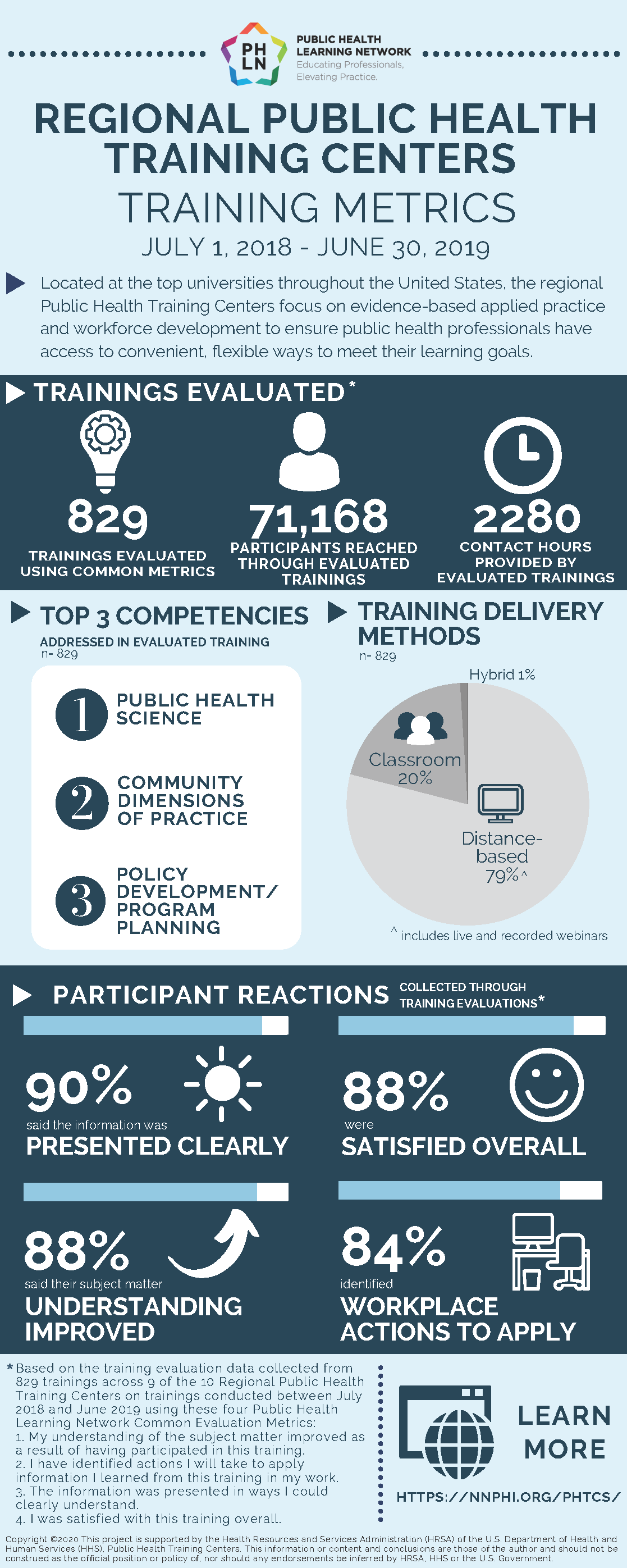
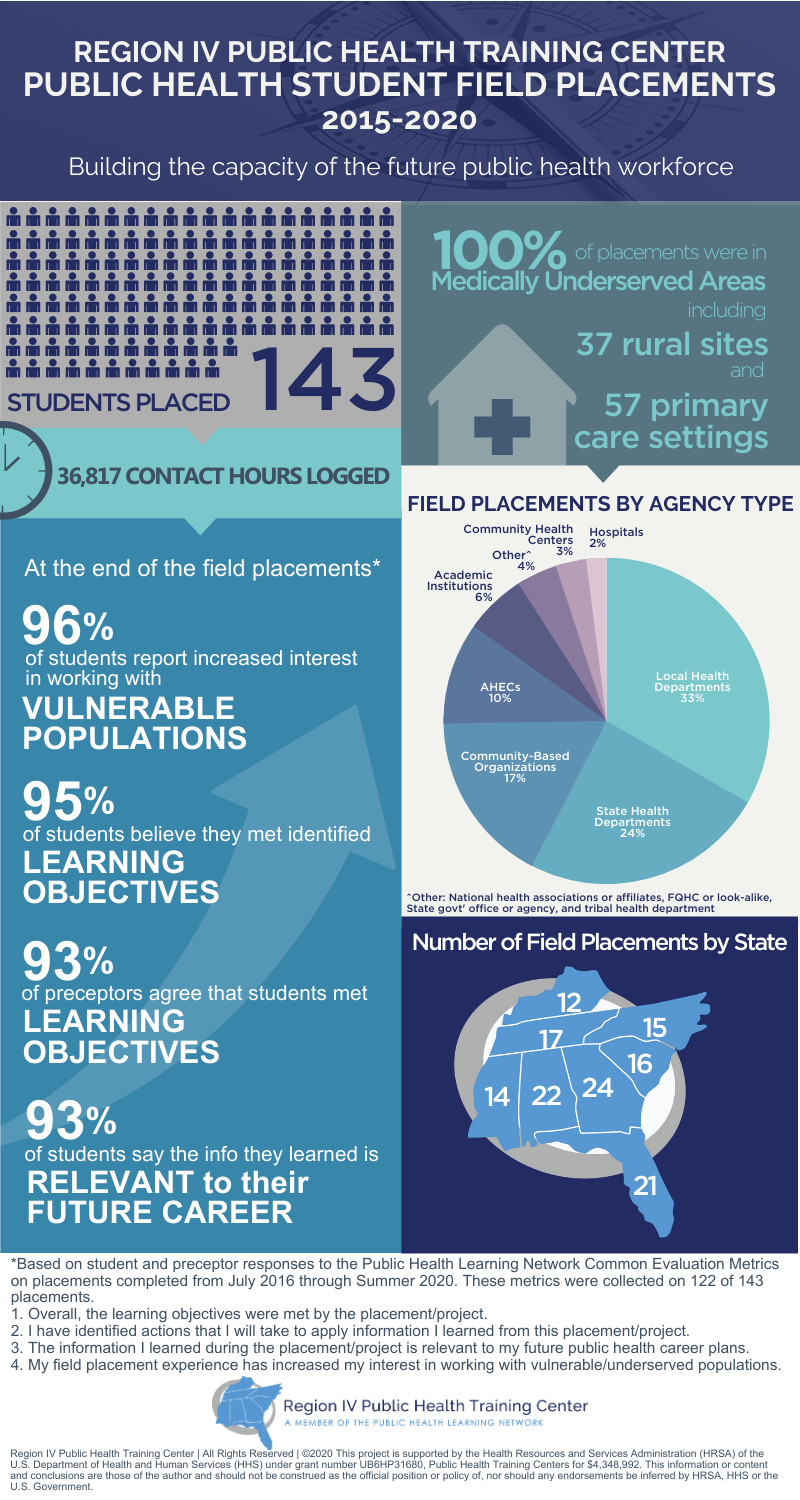
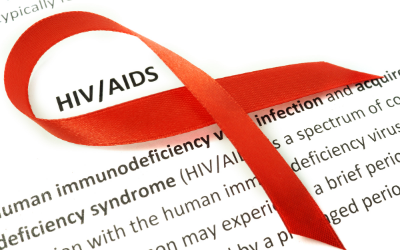
When you participate in a training with the Region IV Public Health Training Center, you become a key part of a national network (the Public Health Learning Network, or PHLN) of ten regional Public Health Training Centers, each funded by the Health Resources and Services Administration to strengthen the public health workforce through education and training.
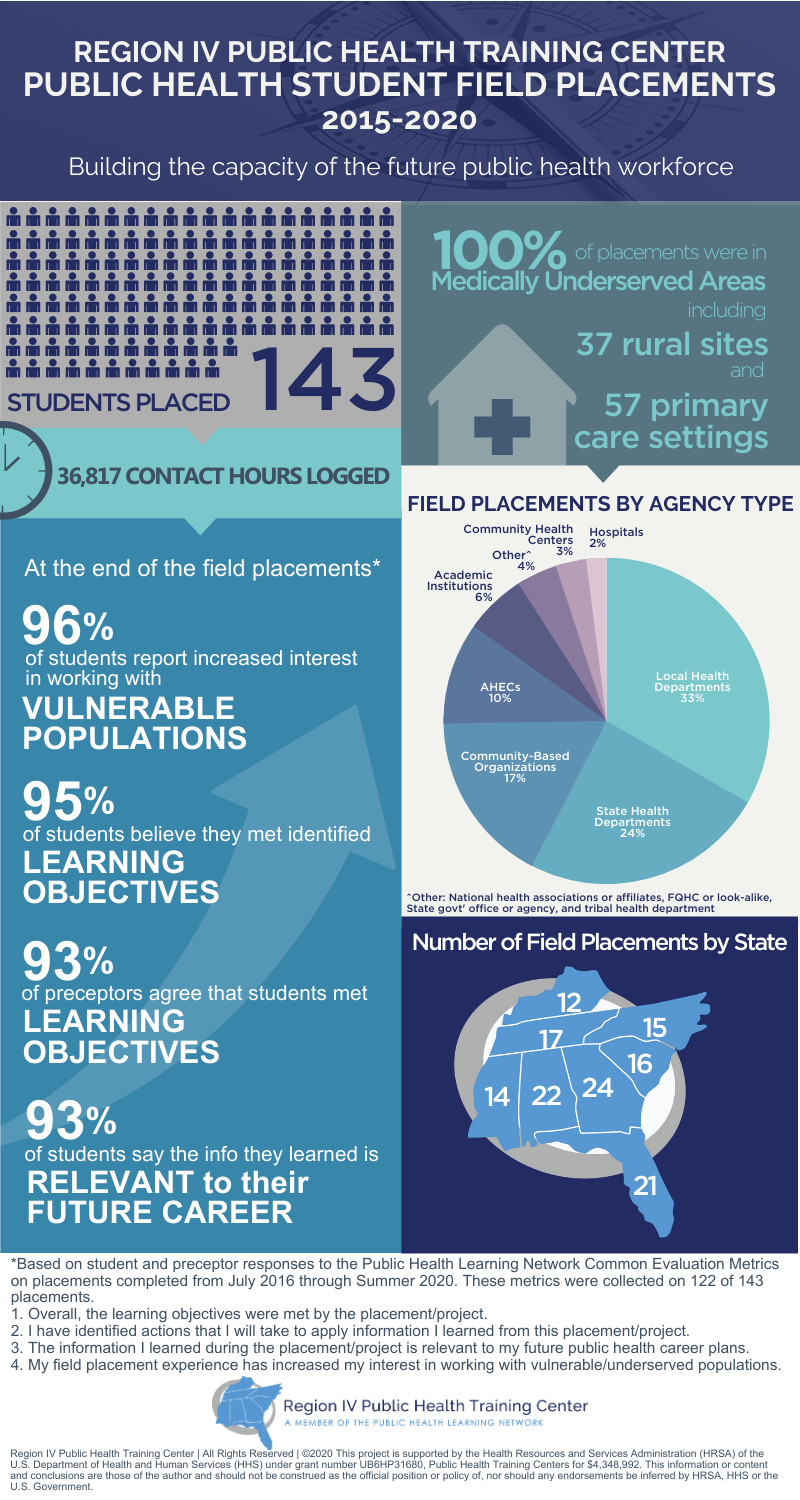
The PHLN is committed to measuring and communicating the influence of our programming. Two new infographics (below) highlight the collective impact and value of the PHTCs activities at a glance. The compiled data highlight the tremendous effort of the PHTCs in designing trainings that clearly communicate relevant public health information in such a way that participants are not only satisfied with the training, but are also able to learn from the trainings and identify actions they can take in their workplace. Likewise, across all regional field placements, the strength and impact of the PHTC field placement program is evident.

by R-IV PHTC | Aug 25, 2020 | Field Placement Stories
Jenesha Nance is an MPH student at the University of South Carolina who served as a Region IV PHTC Pathways to Practice Scholar in the summer of 2019. She worked for SC Thrive, a nonprofit committed to leading South Carolinians to stability by providing innovative and efficient access to quality of life resources.
At SC Thrive, she facilitated benefits trainings, attended outreach events, and supported numerous nonprofits’ partnerships with SC Thrive. She also conducted a needs assessment to help organizations better utilize SC Thrive’s resources, including ThriveHub, a new tool that expedites the government benefit application process and helps connect SC Thrive partner organizations.
Jenesha had the opportunity to work with a wide range of clients, from seniors to schoolchildren. The population she worked with was primarily rural, and issues with transportation, high rent costs, and low income were common. Jenesha explains, “My time with SC Thrive was an eye-opening experience. I learned about real issues those in poverty have. Financial and physical health tie hand in hand. Once a person has all the basic needs such as food, water, shelter and healthcare, they can focus more on building a career, having healthy families, and increasing financial resources.”
“One of the most important skills I gained from my field placement was empathy,” she reflects. “I experienced how those who live in poverty scrape by each day and am grateful for all my privileges. I want to continue in nonprofit work and ensure every person has food, shelter, and healthcare. Then, I can begin to assist people in breaking the cycle of poverty.”
Jenesha is currently completing her last semester at the USC. When the COVID-19 pandemic first hit, she began volunteering with Mutual Aid Midlands to help people access food, housing assistance and utility assistance. She is currently working on a back to school electronics drive to help children access technology like computers and headphones.

by R-IV PHTC | Aug 21, 2020 | Training
Reopening Schools Safely During the COVID-19 Pandemic
Year: 2020 | Competency/Strategic Skill: Change Management | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is 90-minute recording of a webinar held on August 31, 2020.
As the COVID-19 pandemic continues, schools across the country are deciding how to begin the 2020-21 school year, whether for in-person instruction, virtual learning, or a hybrid approach. In this webinar, health and education experts from the Center for American Progress will discuss the current state of school reopenings, considerations for local officials making decisions about reopening, and related health and education research.

by R-IV PHTC | Aug 13, 2020 | Training
National COVID-19 Vaccine Trials
Year: 2020 | Competency/Strategic Skill: Public Health Fundamentals | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 60-minute recording of a webinar held on August 18, 2020.
With dozens of COVID-19 vaccine trials in development and updates changing daily, in this webinar, Dr. Carlos del Rio will discuss a few of the leading COVID-19 vaccine trials, the progress that has been made and next steps in the COVID-19 vaccine trial process. We will also explore the safety and efficacy of the COVID-19 vaccine trial process.

by R-IV PHTC | Aug 13, 2020 | Training
Saving Ourselves: HIV/AIDS and Its Impact on Black Communities
Year: 2020 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: HIV/AIDS | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of an on-demand webinar held on September 2, 2020.
This webinar will focus on the HIV/AIDS epidemic in the Black community and discuss how stigma, disease prevention & awareness, and access to care & treatment play a pivotal role in elimination of the HIV/AIDS epidemic on the national, state, and local level.

by R-IV PHTC | Aug 10, 2020 | Training
Value Based Care 101: Understanding and Preparing for Alternative Payment Models
Year: 2020 | Competency/Strategic Skill: Program Planning | Priority Topic: N/A | Setting: Online | Format: On-Demand | Sponsor: University of North Carolina, Wilmington
Overview:
This is a 90-minute recording of a live webinar. It is the first in a series of two webinars on Value Based Care.
Understand what value-based care is and why there is a value-based care movement. Explore the nationally accepted principles of value-based care. Learn about the philosophy and framework of the HCP-LAN Alternative Payment Model and review the current state of VBC initiatives.
Presented by Michaelle Gady, JD, President and CEO of Atromitos, LLC, Peter Freeman, Senior Consultant at Atromitos, and Sarah Jagger, Vice President of Operations at Atromitos.

by R-IV PHTC | Aug 10, 2020 | Training
Value Based Care 201: Preparedness for the Implementation of VBC Models
Year: 2020 | Competency/Strategic Skill: Program Planning | Priority Topic: N/A | Setting: Online | Format: On-Demand | Sponsor: University of North Carolina, Wilmington
Overview:
This is a 90-minute recording of a live webinar. It is the second in a series of two webinars about Value Based Care.
Value Based Care 201 will be presented by Michaelle Gady, JD, President & CEO of Atromitos, LLC, Peter Freeman, Senior Consultant at Atromitos, and Sarah Jagger, Vice President of Operations at Atromitos. A one hour presentation will be followed by 30-minutes of Q&A.

by R-IV PHTC | Jul 29, 2020 | Training
Police Violence as a Public Health Problem
Year: 2020 | Competency/Strategic Skill: Public Health Fundamentals; Cultural Competence, Diversity and Inclusion | Priority Topic: N/A | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is 90-minute recording of a webinar held on August 10, 2020.
In recent months, we have seen an extraordinary number of people take to the streets to protest police violence and systemic racism. This webinar will focus on police violence as a public health issue, a framework that allows us to view police violence in a broader societal perspective. We will discuss basic measures of police violence across populations and limitations of the existing data. De-funding and abolition will be discussed as possible strategies to reduce police violence.

by R-IV PHTC | Jul 26, 2020 | Training
PPE: What Always Works, What Sometimes Works, What Never Works and Why
Year: 2020 | Competency/Strategic Skill: Public Health Fundamentals | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a one-hour recording of a webinar held on July 30, 2020.
This webinar is co-sponsored by the Alabama Fire College Workplace Safety Training Program and the Deep South Biosafety Worker Training Program.
This webinar will discuss Personal Protective Equipment (PPE) applicable to the COVID 19 crisis. It is assumed that students are aware of standard PPE certification/requirements ( e.g. the US Department of Labor: OSHA standards for both personal and respiratory protection ). This webinar will focus on how to adapt these to the current situation, as well as crisis standards applicable when PPE may be limited/unavailable.

by R-IV PHTC | Jul 13, 2020 | Training
Operational Challenges for EMS during COVID-19
Year: 2020 | Competency/Strategic Skill: Problem Solving | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a 60-minute recording of a webinar held on July 21, 2020. This webinar is co-sponsored by the Alabama Fire College Workplace Safety Training Program and the Deep South Biosafety Worker Training Program.
The COVID-19 pandemic has created numerous challenges for EMS including out-of-hospital management of patients and PPE use by EMS personnel. Dr. Lekshmi Kumar will discuss the operational changes that have been adapted by Grady EMS during the COVID-19 pandemic including changes to personnel and PPE for patient and personal safety, airway management, resuscitation, and cessation when responding to a cardiac arrest patient. Dr. Isakov will discuss best practices in protecting EMS healthcare personnel and strategies for overcoming PPE resource challenges and complacency in the use of PPE by EMS personnel.

by R-IV PHTC | Jul 8, 2020 | Training
Year: 2020 | Competency/Strategic Skill: Program Planning | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a one-hour recording of a live webinar held on July 28, 2020.
This webinar is co-sponsored by the Alabama Fire College Workplace Safety Training Program and the Deep South Biosafety Worker Training Program.
The webinar will discuss COVID-19 in pediatric patients specifically focusing on their pre-hospital management with a target audience of first responders. We will review the epidemiology of COVID-19 in pediatrics, assessment and management of pediatric patients with suspected or confirmed COVID-19, prehospital management of pediatric respiratory emergencies and patients with COVID-19, discuss the emerging illness known at MIS-C, and review prehospital cases of pediatric patients with COVID-19.

by R-IV PHTC | Jul 1, 2020 | Training
Alabama Public Health Training Network COVID-19 Series
Year: 2020 | Competency/Strategic Skill: Program Planning | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-Demand | Sponsor: Alabama Public Health Training Network

by R-IV PHTC | Jun 29, 2020 | Training
Whitefoord Health Equity Webinar Series
Year: 2020 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: Childhood Obesity | Setting: Online | Format: On-Demand | Sponsor: Emory University/Central Office
Overview:
This is a three-part webinar series on health equity co-sponsored with Whitefoord, Inc.
July 7, 2020, 12-1pm ET: Health Equity in Young Children
Disparities in health outcomes begin early in life, and are often the result of social and economic inequities. Many of the health problems children experience are the result of preventable health disparities.
July 23, 2020, 12-1pm ET: Food Insecurity
Food insecurity and a lack of availability and affordability of healthy food affects the health and wellbeing of vulnerable populations. As a community, we must work together toward strengthening and making our food systems more equitable.

by R-IV PHTC | Jun 29, 2020 | Training
Chemical Hazards During COVID-19: Disinfectants, Cleaning Chemicals & Tear Gas
Year: 2020 | Competency/Strategic Skill: Public Health Fundamentals | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on July 9, 2020. This webinar is co-sponsored by the Alabama Fire College Workplace Safety Training Program and the Deep South Biosafety Worker Training Program.
The COVID-19 Pandemic has created numerous challenges to EMS and Healthcare Providers including responding and managing injuries from exposures to cleaning chemicals and disinfectants by patients who are concerned with virus transmission. Additionally, recent protests have raised concerns regarding risks of viral transmission during crowd gatherings, however, injuries from trauma and tear gas have also been reported. During this webinar, two experts in medical toxicology, will discuss hazards from disinfectants, cleaning chemicals and tear gas as well as the emergency assessment and management of associated injuries.

by R-IV PHTC | Jun 23, 2020 | Training
Addressing Racial HIV Disparities Using Pre-exposure Prophylaxis (PrEP) Among Young Adults: Considerations for Practice
Year: 2020 | Competency/Strategic Skill: Cultural Competence, Diversity and Inclusion | Priority Topic: HIV/AIDS | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a live webinar.
African Americans are disproportionately affected by HIV. Reducing HIV rates among African American young adults may produce the most meaningful impact in addressing the HIV epidemic in the US. Pre-exposure prophylaxis (PrEP), a medication regimen to reduce risk of HIV infection, is a promising HIV prevention strategy but its benefits have not been fully realized among African American young adults. This webinar focuses on barriers to PrEP access and uptake among this population and examines approaches to address these barriers. Considerations regarding PrEP during the COVID-19 pandemic will also be explored.

by R-IV PHTC | Jun 23, 2020 | Training
Crisis on Top of Crisis: Guidance for Disaster Shelters during the COVID-19 Pandemic and How to Deliver the Message
Year: 2020 | Competency/Strategic Skill: Problem Solving | Priority Topic: Other Infectious Disease | Setting: Online | Format: On-demand | Sponsor: Emory University/Central Office
Overview:
This is a 90-minute recording of a webinar held on July 2, 2020. This webinar is co-sponsored by the Georgia Hurricane Response Hub.
Preparing for hurricane season can be stressful especially during the COVID-19 pandemic. During this webinar, CDC experts will discuss special considerations for general population hurricane shelters during the COVID-19 pandemic and how community leaders, nonprofit organizations, and public health professionals can effectively communicate messages. They will also share hurricane resources and educational materials you can use and distribute within your own communities.

by R-IV PHTC | Jun 23, 2020 | Field Placement Stories
Jamad Smith is pursuing an MPH at the University of Southern Mississippi to help him prepare for a career in health administration. In early 2020, he was placed at the Mississippi Rural Health Association as a Region IV PHTC Pathways to Practice Scholar.
Initially, Jamad was involved with researching rural hospital access in addition to a performance improvement project on diabetes awareness. Once the COVID-19 pandemic hit, his focus shifted towards the critical role of telemedicine. Jamad was responsible for researching new telehealth guidelines, including billing code updates. He explains, “The coverages basically waived costs of coinsurance and changed the reimbursement provisions based on government guidelines and policy. The goal is for individuals to know that their plan covers testing for COVID-19 and that telehealth is available under their plan.”
Jamad reflects, “This project allowed me to observe how legal and ethical principles played a role in public health decision making with stay at home orders. Telehealth proved its value during this pandemic.” This experience allowed Jamad to think deeply about issues any healthcare administrator must grapple with – access, quality of care, resource allocation.
In addition to growing his professional skill set, Jamad enjoyed the positive work culture at the Mississippi Rural Health Association. He explains, “I was surrounded by great mentors in a comfortable work environment. I was welcomed with open arms and was treated with respect and trustworthiness. I was able to perform meaningful work with every task and nothing I did was pointless or irrelevant.”
Jamad will graduate this summer and plans to work in an administrative position in his hometown of Mobile, Alabama or in the Atlanta, Georgia area.