February is for hearts—including yours!
 Heart disease is still the leading cause of death in the United States—about one person every 33–34 seconds CDC, 2023). And here in the Southeast “Stroke Belt,” cardiovascular deaths remain higher than in other parts of the country (Shikany et al., 2022).
Heart disease is still the leading cause of death in the United States—about one person every 33–34 seconds CDC, 2023). And here in the Southeast “Stroke Belt,” cardiovascular deaths remain higher than in other parts of the country (Shikany et al., 2022).
Every February, American Heart Month calls attention to those statistics and urges communities to protect their heart health (CDC, 2024). At the Region IV Public Health Training Center (Region IV PHTC), we also see this month as an invitation to care for another vital heart: the heart of the public health workforce itself—your motivation, sense of purpose, and connection to this field.
This article is a little love letter to you and your colleagues across Region IV—about what it might look like to fall back in love with public health.
Remember what first captured your “public health heart.”
Most of us didn’t choose public health for the paperwork or the meetings.
You might have been drawn in by :
- A community that shaped you and that you wanted to give back to
- A story about injustice that made you say, “We have to do better than this.”
- A mentor who opened your eyes to the power of prevention.
- Data that revealed a pattern you couldn’t ignore.
Take a moment this Heart Month to consciously reconnect with that origin story:
- Tell it out loud in a team meeting or journaling session.
- Share it with a newer colleague or student—many early-career professionals need to hear why people stay.
- Pair it with the data: in a region where cardiovascular disease deaths are higher than the national average, your work on chronic disease, social determinants, and systems change literally touches people’s hearts (Shikany et al., 2022).
Your “why” hasn’t disappeared—it may just be buried under emails, crises, and constant change.
Notice the signs of a tired public health heart
Just like physical heart disease can be silent, our professional “heart health” can erode quietly over time.
- You feel numb when news breaks about another preventable health outcome.
- You find yourself irritable or cynical about partners, policies, or the public.
- The work feels like an endless to-do list, not a calling,
- You’re so busy caring for everyone else’s health that your own habits—movement, sleep, primary care visits—fall to the bottom of the list.
If any of that sounds familiar, it doesn’t mean you’re failing. It means you’re human, working in a field that has carried extraordinary pressure—especially in recent years.
During American Heart Month, consider doing a quick “check-up”:
- What gives me energy inmy work right now?
- What consistently drains me?
- Where do I feel most connected to people and purpose—and where do I feel most alone?
You don’t have to fix everything at once. Awareness is the first act of care.
Small ways to fall back in love with the work
Re-energizing your relationship with public health doesn’t require a career change or a big grant—often it starts with small shifts.
1. Reconnect with real people, not just problems.
Heart disease statistics can be overwhelming. But your heart might light up when you:
- Visit a clinic, community-based organization, or coalition meeting.
- Hear a patient or community member share how a program changed something tangible in their life.
- Talk with a local partner about what’s working, not just what’s missing.
If you’re mostly behind a screen, consider building in one “people-centered” touchpoint each week—even a short phone call with a partner instead of an email.
2. Let data tell hopeful stories.
In Region IV, we know there are real disparities in cardiovascular outcomes (Shikany et al., 2o22). But there are also micro-victories that get lost in the big picture:
- A county that finally implemented a blood pressure screening initiative
- A cohort of lifestyle coaches who completed training
- A clinic that tested a new workflow to connect patients with community resources
Make time to look for trend lines that bend in the right direction, even slightly. Share those stories with your team. Progress is rarely dramatic, but noticing it can rekindle pride and momentum.
3. Protect the boundaries that keep your heart in the work.
Loving public health doesn’t mean being available 24/7.
This month, experiment with one boundary that protects your energy:
- No email after a certain hour
- A real lunch break away from your desk
- Blocking small “focus” windows on your calendar to do deep work instead of constant multitasking
Boundaries help you stay in this field for the long haul—which is a win for you and for the communities you serve.
4. Learn something that sparks curiosity (not just obligation).
Professional development can feel like one more requirement. But the right learning experience can remind you why you cared in the first place.
Look for trainings that:
- Give you new tools (e.g., communication, leadership, evaluation, or equity frameworks)
- Offer time for reflection and discussion, not just slides
- Connect you with colleagues across other counties or states in Region IV
Even a 90-minute webinar that sparks one “aha” moment can shift how you feel heading back into your workday.
How Region IV PHTC can support your public health heart
At the Region IV PHTC, our mission is to strengthen the public health workforce across the Southeast. That includes skills, but also your sense of connection and purpose.
Through:
- Live webinars and interactive workshops on topics like communication, leadership, evaluation, and systems thinking
- Self-paced online modules you can take when your schedule allows
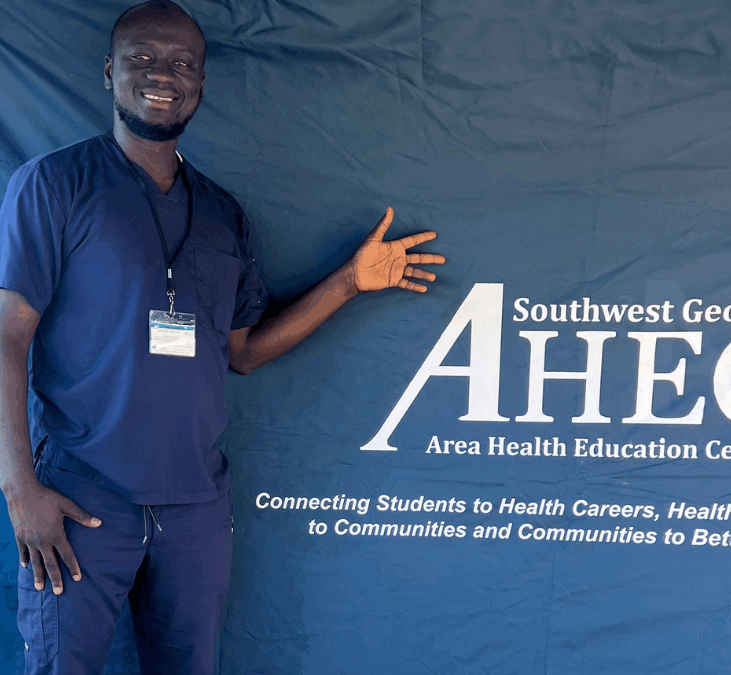
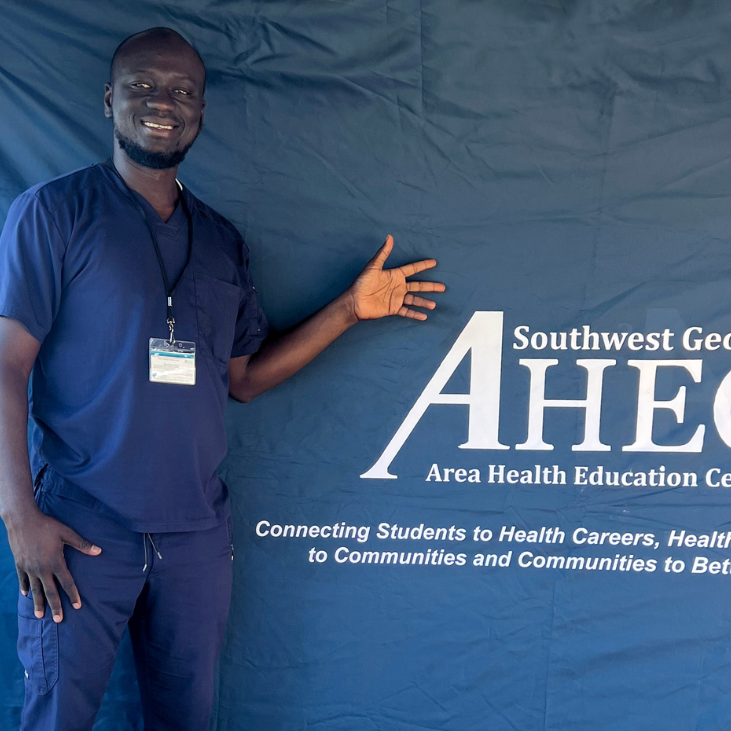
- Leadership development and student programs that bring fresh energy into the field
- Stories and conversations—via podcasts, spotlights, and features—that highlight the real humans behind public health in Region IV
…we hope to give you places to learn, breathe, and remember that you’re not alone in this work.
This American Heart Month, consider:
- Bringing a colleague to a Region IV PHTC training as a shared “reset”
- Sharing one of our resources with a partner who’s feeling discouraged
- Reaching out to a peer in another state to swap ideas and encouragement
Your heart matters, too.
February is a powerful reminder that cardiovascular disease is still our nation’s #1 killer—and that many of the risk factors are preventable (CDC, 2023).
But it’s also a chance to remember that the health of our communities is tied to the health of the people who serve them. Your heart—your well-being, your sense of meaning, your capacity to care—matters just as much as any metric on a dashboard.
Falling back in love with public health doesn’t mean ignoring the very real challenges you face. It means:
- Re-anchoring in your “why”
- Nurturing the relationships and practices that sustain you
- Allowing yourself to see the progress you’re helping create, even when it’s small
From all of us connected to the Region IV PHTC:
Thank you for the ways you show up—day after day—for the hearts of the communities you serve.
This month, we hope you’ll also take a little time to tend to your own. ❤️
Sources:
Centers for Disease Control and Prevention, (2023). Heart disease facts. U.S. Department of Health and Human Services.
Centers for Disease Control and Prevention. (2024). American Heart Month toolkits. U.S. Department of Health and Human Services.
Shikany, J. M., Safford, M. M., Brown, T. M., Durant, R. W., Halanych, J. H., & Levitan, E. B. (2022). Deaths from cardiovascular disease in the Stroke Belt surpass rates elsewhere in the nation. Journal of the American Heart Association.